 Should surgeons who do bariatric surgery on patients traveling considerable distances for care be sanctioned? asks Dr. Arlen Meyers.
Should surgeons who do bariatric surgery on patients traveling considerable distances for care be sanctioned? asks Dr. Arlen Meyers.
Or should facilitators and surgeons do better screening of medical tourists and provide comprehensive care management?
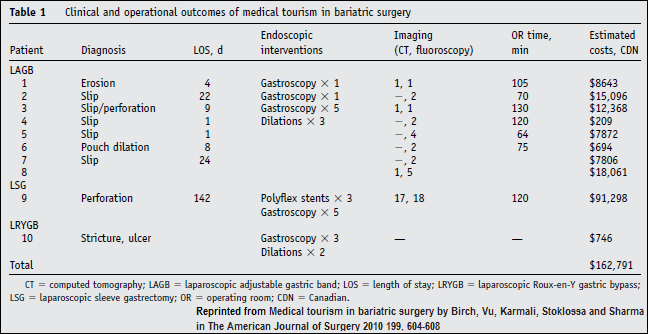
Three doctors in Edmonton, Alberta, writing in the American Journal of Surgery, describe their experience with 10 bariatric surgery patients who had had weight loss operations away from home.
Their conclusions:
- Medical tourism for bariatric surgery will continue to grow.
- New management algorithms may be needed to treat this patient population because they “undoubtedly will require the expertise and care of a bariatric surgical team at some point in their lives and, as such, will continue to burden the limited resources currently available.”
- A medical tourism approach to the surgical management of obesity is inappropriate and raises clear ethical and moral issues.
Their paper, Medical Tourism In Bariatric Surgery, prompted Dr. Meyers to ask his question in a LinkedIn group.
We agree with their first conclusion. Weight loss surgery medical tourism has a very good future.
Bariatric surgery medical tourists need long term care management
As to their second conclusion, we believe that all involved – patients, agents, surgeons and care managers – need to understand the long term needs of these patients and integrate long term care management into bariatric surgery medical travel programs. Follow up of these patients should be seen not as a burden on scarce resources but as an extension of a good health care program that embraces choice, even if the choice is to go abroad for surgery.
Their third conclusion, that a medical tourism approach to the surgical management of obesity is inappropriate and raises clear ethical and moral issues, is not supported by the data they present.
Complications of weight loss surgery
The Canadian surgeons reviewed 10 cases that had come to them with problems caused either directly or indirectly, from their weight loss surgery. All had had surgery outside of Alberta (Canadian government health care is structured through each province), but they do not say where these patients actually had their surgery. They do not say who of those 10 went elsewhere in Canada, traveled to the US for surgery, or traveled to a further away medical destination.
While the authors imply these patients received a lower quality of surgery, this may not be the case. The problem may not at all be one of “medical tourism” but patient education and/or patient compliance.
Gastric banding surgery for medical tourists
8 of the 10 patients had gastric banding surgery. What the authors highlight as the problems for medical tourists after this surgery are important evidence that reveal the sort of treatment planning and care management required for such medical travelers.
The one patient who had Roux-en-Y surgery had what might be considered a routine complication. Its resolution was simple and inexpensive and required no surgery. She was rehydrated, medicated, given vitamins, and sent to a bariatric dietitian.
The one patient who had gastric sleeve surgery had major complications. The authors suggest her troubles were due to the initial bariatric surgery yet they may just as easily have been caused by the follow up surgery in the US.
Her case: she experienced abdominal pain while flying to the US on vacation (we are not informed how long after the surgery the patient went on the vacation). While abroad, she eventually sought medical attention for the pain, had corrective surgery, developed severe sepsis, had further surgery followed by intensive care. She returned to her home in Canada when she was deemed stable.
More screening for gastric banding surgery medical tourists
The evidence the authors present of complications that the remaining 8 of the 10 patients had after their gastric banding surgery is instructive.
They describe gastric banding patients who came to them seeking relief from typical complications of this surgery including slippage of the band, erosion, and obstruction. Gastric banding clearly requires more ongoing care management over time. It is more vulnerable to patient non-compliance.
The evidence they present about gastric banding outcomes supports a policy my medical travel company, Cosmetic Surgery Travel, put in place many years ago. We do not accept medical travelers who want gastric banding unless we can verify independently that they have a qualified surgeon or primary care physician at home who knows they are having the surgery abroad and will help monitor their progress over time once they return.
We have learned, too, that surgery for some very obese patients (BMI>45) requires a few extra steps and/or surgical tools and care, and we have specially selected a few hospitals and surgeons to work with for these patients.
 >
>
One Response to Should Medical Travel Bariatric Surgery Doctors Be Sanctioned?